In the past years, we have seen impeccable advancement in medicine. Indeed, this field has come a long way. Conditions that were usually considered lethal are now treated easily. Pandemics that killed thousands and millions are now small infections that don’t require serious attention.
Similarly, organ replacement and transplantation have changed the concept of life. Cardiac arrest was once a major cause of death worldwide. But now, thanks to the untiring efforts of medical engineers, this condition can also be reversed.
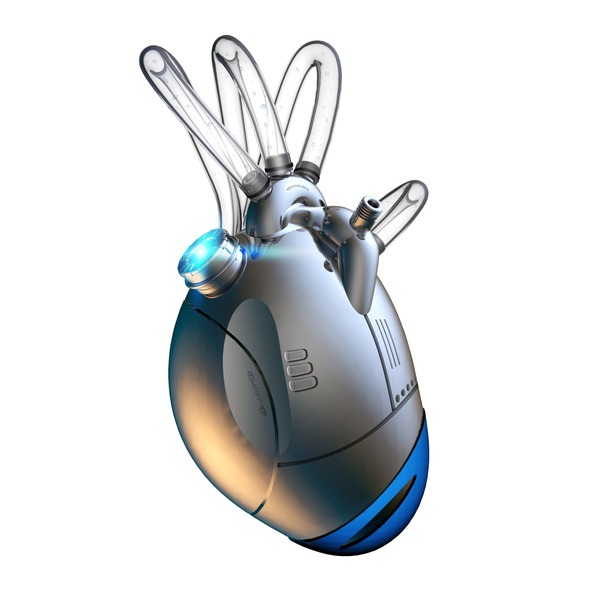
We have not only made medications but replacements too. From letting a person die because of medical insufficiency to now replacing the non-functional heart with a small piece of machine, it was indeed an evolution. But this journey wasn’t easy. The artificial heart that seems to be a piece of cake right now took a long process to develop. After dozens of prototypes and failed experiments, we finally have something we can appreciate and use.
If you want to learn more about this device that can replace a human heart, then stick till the end. In this article, we will explore the history of the artificial heart while covering all the facts and details about it. Let’s get started.
The First Theory for Artificial Heart
For the very first time, the idea of an artificial heart or blood support system was proposed in theory by Julien Jean Cesar LeGallois. This theory was put forward in 1812, but the practical work started in the 1920s.
It was only a unique fantasy until an inventor named Charles Lindbergh decided to work on this mission. He traveled all across the world and finally teamed up with a surgeon named Alexis Carrel to seriously work on an artificial heart.
They both worked tirelessly and invented the concept of temporary heart support, which made open-heart surgery possible in the first place. This was a big step in cardiology, and due to their exemplary work, they received Nobel Prize for their efforts.
First Trial of Total Artificial Heart
The efforts of Carrel and Lindbergh opened up the gates to innovation in this field. Many years later, in 1937, Dr. Vladimir came up with an idea of a total artificial heart.
It was very different than the first temporary blood pumping system. Because as opposed to providing support for temporary means, it was meant to be a permanent replacement of the heart.
When he was developing it, he came across many failed versions. But then after several tries, he finally made a machine that he could experiment on. And for the very first time, it was put on a dog who survived for 5 hours, post-surgery.
If you think about it, the machine was a failure. But in a way, it proved that it was possible to build a functional artificial heart.
The Famous Lung Heart Machine
Two years after the failed experiment of the total artificial heart, a patient lost his life during surgery. Even though his heart had support, there was no way for gaseous exchange as his lungs were detached from the heart. This patient wasn’t unique because many other lives were lost due to the same reason. But unlike other doctors, the surgical team of this patient decided to stop this vicious cycle.
After this case, Dr. Demikhov produced a machine that could not only support the heart but also provide a gaseous exchange facility to the patient as well. This ensured that the patient wouldn’t collapse in between surgery, and longer operation started to take place with significant ease. This is how the famous heart-lung machine was introduced in the market.
It took a lot of time to make this device, but the results were worth it. From 1953 until now, this machine has been modified several times. But it has proved to be a lifesaver for many patients. In the market, it is known as Mayo Gibbon Type Oxygenator.
Efforts for Total Artificial Heart
Even though the first total artificial heart wasn’t perfect, its idea still proved to be a remarkable effort. And after Dr.Vladimir, many other doctors came forward with their versions of an artificial heart.
Some remarkable examples include the work done by Dr. TetsuzoAkutsu and Dr. Willem Kolff, whose model worked for 1.5 hours. Similarly, Domingo Liotta produced his version of TAH, which worked for 13 hours.
But Liotta was different from the rest. He didn’t stop with his unsuccessful experiment. He continued the journey and kept improving his TAH, and in 1969, his work was tested on a human being. At first, it was a success, but after 64 hours of function, the condition of the patient started to decline. The pumping capacity of the mechanical heart wasn’t enough for the patient’s needs. Therefore, a human heart transplant was arranged to save him.
But the point to note here is, the doctors realized that it was possible to carry out blood circulation in a human body using a machine. The artificial heart by Liotta was the very first time when a human heart was successfully replaced with an electronic device.
Invention of AbioCor
Another important invention in the field of cardiology includes AbioCor. It was the first artificial heart that could be used without external help. Of course, it had batteries that needed charging, but other than that, it was great. FDA approved it to be used, but only when there was a bi-ventricular failure. Meaning, it could only be applied to a patient whose ventricles weren’t working at all.
Until now, it has been used on only one patient, and that patient died due to complications. Thus, one can say that even though it was better concealed and provided ease of movement, it lacked functionality.
Development of Syncardia Temporary
A device named Jarvik 7 was introduced in 1982. It was an air-pumping machine that could copy the mechanism of the human heart, efficiently. Unlike previous tries, this was made with utter attention to details. That is why the FDA approved it for clinical trials.
Three patients received this machine, and even though they all expired, they still managed to survive for some time. The complications in each patient were different, ranging from pneumonia to multi-organ failure. Because Jarvik7 was a common denominator, it was rejected as well.
But the workers behind this model didn’t lose hope in their work. They kept working on Jarvik 7, and finally, in 1991 they relaunched it with a new name, Syncardia Temporary. They got FDA approval to use this machine as a bridge to a heart transplant, which means when a patient had no other option but a heart transplant, they were put on this device until a donor was arranged. It was a temporary setup, but it was better than leaving the patients high and dry.
The Syncardia Freedom
In 2010, the company holders of Syncardia launched Syncardia Freedom. This device basically allows the patient to get discharged from the hospital and live his life somewhat normally. With this setup, the patient has to carry a 13-pound machine with him at all times to keep his heart pumping. But at least he gets the chance to get out of the hospital bed.
Final Words
From storing organs in an icebox to now using machines as organs, we have done some great work in the field of medicine. The subject of artificial heart has always been a big deal in the medicinal world. Considering the rate of fatalities due to cardiac problems, it is not surprising to see the eagerness of the workers in the cardiology department.
For decades, biomedical engineers have invested their lives to create a machine that can save people. Because even though the human heart transplant is a great option, the donor to recipient ratio is too high. There aren’t enough people who can give their hearts to others. Also, the patients who do receive a new heart, mostly die due to various complications.
In such conditions, creating an artificial heart only makes sense. Until now, we’ve seen many versions of this machine, but the ones that have been used readily include Syncardia freedom and Syncardia temporary. On the other hand, a lung-heart machine is most commonly used in open-heart surgeries.
With the enormous speed of advancement, who knows, maybe one day, we will find a better replacement for the human heart. Till then, we can work on our health and try to prevent conditions that can lead to the need for heart replacement.